WHAT IS OSTEOPOROSIS?
It’s not easy, but every now and again, you can get Ben Philipson, the creator of the Curatron systems to actually sit down and share some of his extensive knowledge on Pulsed Electromagnetic Field Therapy. The article below provides a lot of background material for those of us looking for help with Osteoporosis.
Jump to the PEMF Treatment Section << CLICK HERE >>
The currently accepted definition of osteoporosis is “systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture risk”.
The bone mineral can be measured with reasonable accuracy and precision. These tests form the basis for the diagnosis of osteoporosis and the prediction of fracture risk.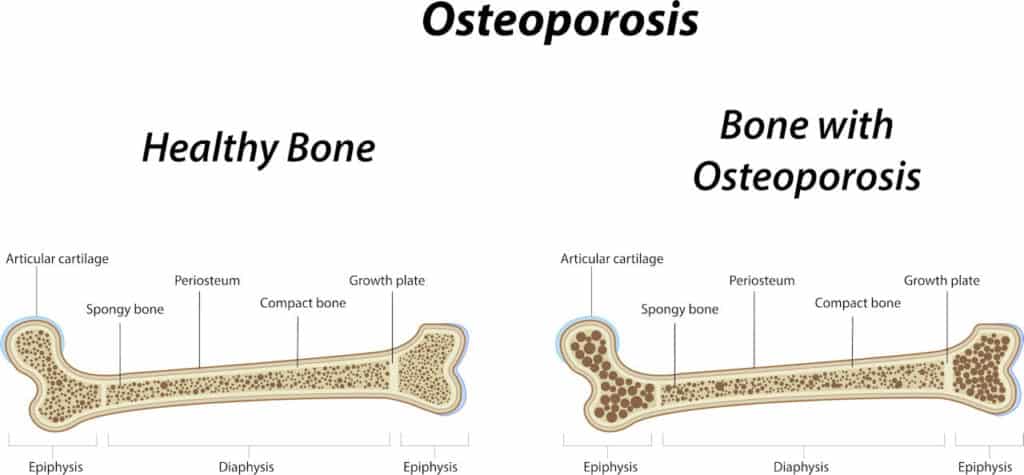
Bone mass refers to the amount of bone tissue contained in the skeleton. Bone mass can be expressed in terms of bone mineral content (the total grams of bone mineral within a given area of bone) or concerning bone mineral density (the bone mineral content normalized for the projected area).
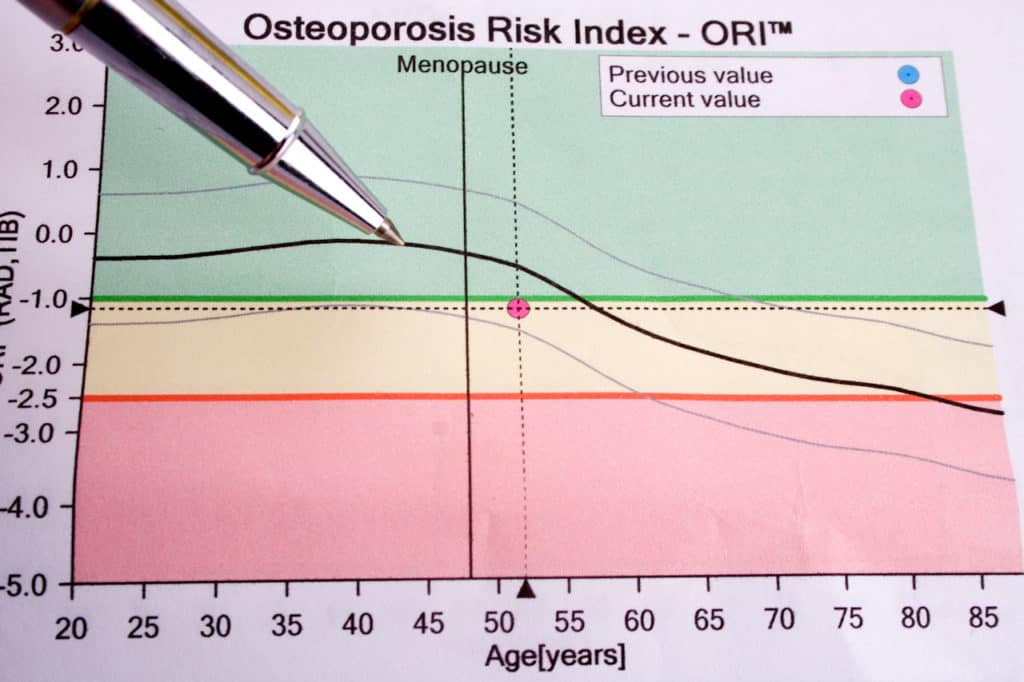
Normally bone density peaks between the ages of 30 to 40 and in subsequent years the bone density decreases. If the decrease is significant enough, the so-called “fracture threshold” is reached.
At this level of bone density, the patient is at significant risk of fracture. These thresholds are reached at different ages, and the extent of bone loss varies depending on the peak bone mass and generic and environmental factors, including activity level and diet.
The decrease of bone density in post-menopausal women is significantly greater than in pre-menopausal women or men. The average annual bone loss in post-menopausal women is 1% – 2% and in men 0.2% – 0.5%. Although the rate of bone loss in women is the highest in the years after the menopause, it continues in many patients for many years and increases again after the age of 70. Annual losses can even reach 3% -5% during the first years following the menopause.
 In women, the major cause of bone loss and osteoporosis is estrogen withdrawal, most commonly associated with the menopause and declining ovarian function, but any cause of estrogen deficiency can cause bone loss.
In women, the major cause of bone loss and osteoporosis is estrogen withdrawal, most commonly associated with the menopause and declining ovarian function, but any cause of estrogen deficiency can cause bone loss.
In men, androgen might play a role in causing osteoporosis.
Here progressive loss of bone starts around the third decade and continues during life.
There are many conditions other than estrogen or androgen deficiency that cause bone loss, including malignancies, metabolic abnormalities, gastrointestinal diseases and exposure to certain drugs. Also, smoking and the excessive use of alcohol may contribute to bone loss.
A study group of the World Health Organization (WHO) has proposed diagnostic guidelines for interpretation of bone-mass measurement in Caucasian women.
Bone density values in individuals are expressed in relation to a reference in Standard Deviation (SD) units.
This reduces the problems associated with differences between the various measuring instruments; it does, however, require defined “normal” ranges.
If bone mineral density (BMD) is below 1 SD but not below 2.5 SD of the mean value of peak bone mass in normal young women, then there is a low bone mass (Osteopenia). If this value is greater than 2.5 SD below this value the patient has Osteoporosis.
This definition is not perfect but it is reasonable for diagnostic and therapeutic considerations.
Osteoporosis is asymptomatic until a fracture occurs.
The risk of fracture is inversely related to bone mass. As bone mass decreases, the risk of fracture increases.
Even relatively small alterations in bone mass can lead to significant changes in the risk of fractures.
The most common sites of fracture in osteoporotic patients are the vertebrae, the hip, and the forearm.
Osteoporotic fractures are associated with significant morbidity and mortality. The most important complaint of patients with osteoporosis is acute or intermittent back pain following normal activity. The pain usually lasts a few days or weeks and then subsides. Such episodes recur and may result in a chronic backache. The episodes are due to crushing fractures of vertebrae. As the disease progresses, loss of height, spinal deformity and fractures occur.
Hip fractures, in particular, frequently have a grim prognosis.
The mortality rate of osteoporotic hip fractures is between 15 % and 20 %, primarily due to pulmonary emboli, pneumonia, and other complications of surgery and prolonged hospitalization. The lifetime risk of hip fractures in white women is as great as the risk of breast, endometrial and ovarian cancer combined. One-half of patients who survive a hip fracture are unable to walk unassisted and 25 % are confined to nursing homes. In up to 20 % of hip fractures, the patient dies within 6 months.
A GROWING HEALTH PROBLEM.
Osteoporosis is a major and growing health problem worldwide.
It affects an estimated 75 million people in the United States, Europe, and Japan, including a large number of men. One-third of women over 65 will have vertebral fractures, and 90 % of women over the age of 75 have evidence of osteoporosis.
The enormity of this health problem when considering the increasing population of elderly people in the world is contrasted by the present therapeutic difficulties in significantly adding bone and improving bone strength once it has been lost.
Osteoporosis will become an even more serious public health problem.
Osteoporosis-related fractures can be expected to double during the next 5 decades. It is also expected that the occurrence of osteoporosis in men will increase.
DIAGNOSIS.
 To be able to diagnose osteoporosis, it is necessary to measure the patient’s bone density. Some techniques are available for this purpose.
To be able to diagnose osteoporosis, it is necessary to measure the patient’s bone density. Some techniques are available for this purpose.
Single- and Dual Photon Absorptiometry.
Single photon absorptiometry (SPA) was initially developed in 1963. This technique involves passing a focused beam of radionuclide radiation across the arm. Because radiation is blocked more by denser tissue (bone) than by soft tissue, bone density can be deducted from these differences.
The disadvantage of this technique includes the requirement for uniform soft tissue around the bone to be measured. Also it is not possible using this technique to measure bone density of hip and spine, being the sites more vulnerable to fractures.
SPA has provided however important population-based information in epidemiological studies, specifically on the effects of aging of the skeleton.
A more sophisticated version of the same technology used in SPA is dual photon absorptiometry (DPA).
It was developed in the early 1970s. The first systems became commercially available in 1980.
DPA uses a radioactive isotope, which emits radiation at two different energy levels, instead of the single energy level used for SPA measurements.
While the body is scanned, the two energy levels are detected and used for mathematical calculations to obtain different values for the different amounts of transmissions of the energy through the body. By using this method, more accurate bone density values are obtained.
Single Energy X-ray Absorptiometry.
Instead of using a radionuclide photon source as in SPA an X-ray source is used in Single Energy X-ray Absorptiometry (SXA). This method can however not be used in spine and hip.
Dual Energy X-ray Absorptiometry.
In 1987 Dual Energy X-ray Absorptiometry (DXA or DEXA) was introduced. Today DXA equipment is widely available and this method is the choice for bone density measurements.
The basic technique of DXA is essentially the same as in DPA except that the radionuclide source is replaced with an X-ray source. DXA has several advantages over the older absorptiometry methods. Measurements take less time, expose the patient to less radiation and most important the results of the measurements are more precise. With the development of p-DXA technique, it became now possible to measure reasonable accurate the density of the forearm, both mid-distal and ultra-distal during the same scan.
Radiographic Absorptiometry.
Bone density is determined from X-ray films by reference to a metal calibration wedge placed alongside the hand during an X-ray procedure. Radiographic densitometry is then used to correlate to bone density measurements. This technique is however outdated.
Quantitative Computed Tomography.
Quantitative Computed Tomography (QCT) represents a modification of conventional CT scanners. The image produced by CT is generated by computer analysis of numerous X-ray transmission values obtained in different directions. The X-ray source and detector rotate around a patient in a fixed plane. From these CT scans bone density is calculated by reference to the density of calibrated phantoms.
Radiation exposure is substantially higher than the other bone density measuring techniques. This form of measurement is useful in elderly patients who may have age-related osteoarthritis and aortic calcification interfering with absorptiometric measurements.
Quantitative Ultrasound.
Over the last few years, various new machines have been introduced for the assessment of skeletal status. By means of Quantitative Ultrasound (QUS), measurements are performed at patella, heel bone, tibia, and ulna. Mainly the Broadband Ultrasound Attenuation (BUA) and Velocity or Speed Of Sound (SOS) are calculated. The systems yield quantitative results averaged over the measurement area the Quantitative Ultrasound Index (QUI) and some calcaneal systems also generate an image. Ultrasound systems have the advantage of obtaining information without the need for ionizing radiation, however, in comparison, the amount of radiation emitted by modern p-DXA systems is extremely low. The main reason for purchasing an ultrasound system is the lower price and portability of these devices compared with p-DXA machines.
Long-term studies of QUS changes over time are still limited. Expressing measurement results on a percentage level is misleading because of the different units and calibrations employed. Studies indicate that standardized precision errors of QUS approaches are at least two times larger compared to corresponding DXA results.
Since this technique is not deriving absolute data on bone mineral density, QUS can be used only for fracture risk prediction.
Laboratory.
Chemical measurements of blood and urine by biochemical screening assays (bone markers) are used to evaluate bone resorption and formation. Although biochemical screening assays have improved over the last few years, they still have an accuracy error of up to 30%.
They are only useful for studying bone turnover in large groups of patients where individual errors are statistically compensated.
Chemical analyses such as urinary hydroxyproline and Pyridinoline crosslinks or serum alkaline phosphatase cannot be used to diagnose osteoporosis. Most of the time they cannot be used to evaluate an imbalance between formation and destruction of bone. They are however used to determine bone turnover and consequently to identify those patients who are likely to be fast bone losers.
DRUGS.
Given the magnitude of the problem of fractures with associated reduced life expectancy, quality of life and last but not least the enormous costs for healthcare providers involved, the most logical approach is prevention.
Bone is continuously turned over by modeling and remodeling, the rates of which are under the hormonal influence. There are some indications that the higher the rate of bone turnover, the higher the rate of bone loss. If women with a high turnover lose more bone over a prolonged period, they should eventually sustain more fragility fractures.
Low calcium intake is a risk factor for fracture, especially in advanced age. Beyond the age of 70 it correlates with low bone mineral density. Since calcium absorption lowers with age, the danger of negative balance increases with age. By assuring sufficient calcium intake, the prognosis of osteoporosis might improve.
Low calorie and low calcium and low protein intake are related to low bone mass density and increase fracture risk. Also, low vitamin D levels are related to low bone mass density specifically in the hip. Vitamin D deficiency is frequent in the elderly, specifically in residents of old age and nursing homes, where nutritional intake and the amount of sunlight may be insufficient.
After the age of 70, mobility decreases twice as much as general health. Physical activity is of high importance for bone mass density in the elderlies.
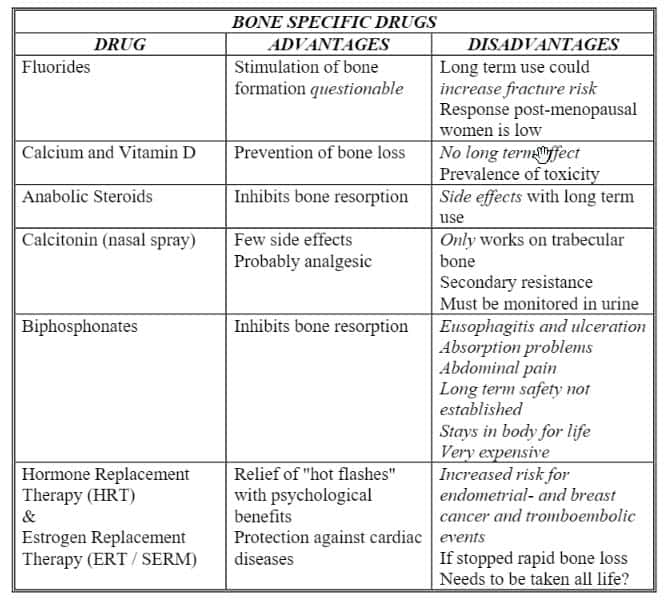
Bone-specific drugs.
Calcium and Vitamin D have no significant long-term effects.
Additional intake of fluorides was thought to be effective to increase bone density. Recent studies have however shown that the effects are no different from calcium and vitamin D for the prevention of fractures in osteoporotic patients. It might even result in less flexible bone structures and thus actually increase the fracture risk.
Anabolic steroids have been used for many years in the treatment of osteoporosis. They probably act mainly by inhibiting bone resorption. They continue only to be of interest for the elderly with advanced disease due to their side effects in long-term use.
Calcitonin inhibits bone resorption and may reduce fracture frequency. However, since calcitonin mainly acts on the trabecular bone (the spongy bone) its effect on bone mass density cannot be established. Its effectiveness on the hip bone is thus questionable.
Bisphosphonates (Clodronate, Alendronate, Etidronate, Olpadronate, Pamidronate, Risedronate, Tiludronate, Ibandronate, Zoledronate) act by inhibiting bone resorption. They decrease the speed of bone loss and fracture frequency. They do have substantial side effects and long-term safety profiles of bisphosphonates are yet to be established. One of the most prominent drugs in the Alendronate group is a very expensive drug (Fosamax), hard to use, rough on stomach and throat, including ulceration and bleeding.
Hormone Replacement Therapy (HRT & ERT). Estrogens are widely used for post-menstrual osteoporosis treatment. Specifically, the psychological benefits (relieves hot flashes) and their possible protection against cardiovascular diseases, is attractive. However, it might be necessary to use them throughout life. They are poorly accepted by women over 70 years. If discontinued after prolonged use accelerated bone loss will occur.
Selective Estrogen Receptor Modulators (SERM) produces both estrogen-agonistic effects on bone and lipid metabolism and estrogen-antagonistic effects on uterine endometrium and breast tissue.
New drugs for osteoporosis will require fundamental advances of knowledge in this field. The current most widely used treatments drugs were developed essentially without fundamental in-depth understanding. Estrogen, bisphosphonates, and calcitonin are mainly used therapeutically as bone resorption inhibitors.
BONE METABOLISM.
The calcified mass of adult bone has three types of surface.
- A surface on which nothing seems to happen. This includes about 90 percent of the bone surface.
- A surface on which bone is being formed.
- A surface at which bone is being resorbed.
Bone formation and bone resorption go on continuously and simultaneously throughout life, though the rates change with age and vary in different parts of the skeleton.
Osteoporosis occurs when bone resorption is greater than bone formation. Bone formation comprises two steps, the laying down of the extracellular matrix and the deposition therein of bone salt.
The dynamic processes of formation and destruction of bone are under cellular control.
Bone formation is controlled by single nuclear cells called Osteoblasts, and bone resorption by multinuclear giant cells called Osteoclasts. Bone is a specialized connective tissue in which a matrix consisting of collagen fibers, a large variety of other proteins and ground substance is impregnated with a solid mineral.
The bone matrix is responsible for the resistance of bone to tractional and torsional forces. The collagen forms more than 25 % of the bones and is synthesized by osteoblasts.
On the bone surface, collagen fibers are normally arranged in concentric rings of the hard calcified matrix.
The bone minerals provide the bone compressive strength and rigidity. It contains the mineral salts hydroxyapatite and calcium. Also, there are small amounts of magnesium hydroxide, fluoride, and sulfate.
As these salts are deposited in the framework formed by the collagen fibers of the matrix, crystallization occurs, and the tissue hardens. This process is called calcification or mineralization. Both the concentrations of ions of calcium and phosphate in the extracellular fluid maintain crystallization. If the concentration is not adequate, the tissue will not be hard enough resulting in increased bone fracture risk.
There are two types of bone structure: cortical (compact) bone and trabecular (spongy) bone.
Cortical bone is denser and constitutes 80 % of the skeletal mass and forms the external layer of all bones in the human body.
Trabecular bone consists of lamellae arranged in an irregular latticework of thin plates of bone and helps long bones to resist the stress of weight placed on them.
The process by which bone forms is called ossification.
Bone forms either by the mineralization of cartilage or directly by osteoblasts in a collagenous matrix.
During the first two decades of life bone grows, followed by consolidation and reaching its peak value around thirty-five years. After this peak, bone loss starts. Nutritional factors, especially calcium intake, the level of physical activity and generic factors are important in determining the peak bone mass.
When a bone is fractured, it heals with bone. Bone is the only solid tissue in the body that can replace itself.
Bone healing is simple when it occurs smoothly, complicated when it does not. The process is being initiated by stimuli from the bone itself. Fractures through bone with a good blood supply, surrounded by muscle and without soft tissue trauma, have an excellent chance of healing, but fractures at the middle of long bones, particularly with extensive soft tissue damage, have a high incidence of non-union.
PULSED ELECTROMAGNETIC FIELD TREATMENT
Selected low-energy time-varying electromagnetic fields have been used during the past 15 years to treat un-united fractures (non-unions). More than 100,000 patients, mainly in the USA, have been treated.
Retrospective studies have substantiated their biological effectiveness in large numbers.
Bone is responsive to the mechanical demands placed on it. When loading diminishes, as it does during bed rest, immobilization and weightlessness, bone mass is lost.On the other hand when loading is increased correctly, bone mass increases.
Results of biomechanical and histologic investigations prove that electromagnetic fields not only prevent bone loss but also restore bone mass, once lost.
A program was set up at the McGill University of Montreal, where was found that electromagnetic fields damp bone resorption activity. Furthermore prove was found that selected electromagnetic fields increase bone formation.
The resorption of bone is lowest and formation of new bone greatest when the energy of the imposed fields is concentrated in the lower frequency components.
These results are consistent with other studies showing, that cells respond to a broad spectrum of frequencies. They appear to be most sensitive to frequencies in the range of those produced endogenously, that is in the range of 1000 Hz or less. Tissue dosimetry studies show that the frequency response of cortical bone over a range of 100 Hz to 20 kHz show a steep roll off between 100 and 200 Hz.
Electro-magnetic fields at specific frequencies have shown to produce osteogenic effects in a turkey ulna model. Furthermore, low-amplitude signals decrease bone resorption in a canine fibular model.
Lifestyle factors like malnutrition, smoking, excessive use of alcohol and a sedentary lifestyle contribute to and worsen, osteoporosis.
It is not known whether this response derives from decreased osteoblastic activity, increased osteoclastic resorption, or both.
Elderly persons can heal fractures in normal intervals, showing that osteoblasts can be activated by appropriate stimuli.
A pilot study at the Pacific Health Research Institute in Honolulu was designed to provide concrete data on the restoration of bone mass in postmenopausal females. A total of 20 subjects between 57 and 75 years, all with decreased bone mineral density as defined by a bone densitometer, were treated during 12 weeks. After 6 weeks, the bone density rose in those patients with an average of 5.6%.
Electromagnetic fields do modify biological behavior by inducing electrical changes around and within the cell.
The key to the rational use of electromagnetic fields lies in the ability to define the specific treatment parameters (amplitude, frequency, orientation, and timing).
Various studies have clearly shown that bone density does increase in osteoporosis-prone patients exposed to specific pulsed electromagnetic fields.
Properly applied pulsed electromagnetic fields, if scaled for whole body use, have clear clinical benefits for treatment of osteoporosis.
Some postings you may enjoy:
There is more to learn!
Amjo Corp has been working with Curatron systems for nearly two decades. Our first sale of a Curatron PEMF system was in May of 2000. Our experience and knowledge are second to none. Call us and find out!
The information at this website including the science pages, doctor's letters and the testimonials from our customers are not meant to imply that you will receive similar or identical results. It is very important that you do independent research before ordering a Curatron 2000 product. The information provided in this website is not medical advice. Readers are encouraged to obtain the help, services, and recommendations of doctors and other licensed medical practitioners. The webmaster and none of us at Amjo Corp are not medically trained and we are selling this product as a business and for profit. In the USA, the Curatron 2000 series have not yet been granted FDA approval as a medical device. Please read and heed all the information provided by your doctor and in the manual provided with the products we sell. We strive for accuracy. It's possible that there are errors on this website, you the web visitor should take the time to perform thorough research independently of this web site, Amjo Corp and Curatronic Ltd. cannot be your sole source of information. We encourage you to do independent research of this technology. Please do not use this website as your sole source of information for PEMF Technology. Outside the USA pulsed magnetic field therapy (PEMF) has been approved in some countries, by health authorities as medical therapy for human applications. In the European Community the Curatron devices are certified as medical devices according to the Medical Device Directive 93/42/EEC. The devices are manufactured according to ISO 13485 for Good Manufacturing Practice.